Gout, long considered simply a painful joint condition, casts a shadow far beyond the physical realm. For men who experience this inflammatory arthritis, the impact on mental health can be profound and often overlooked by both patients and healthcare providers.
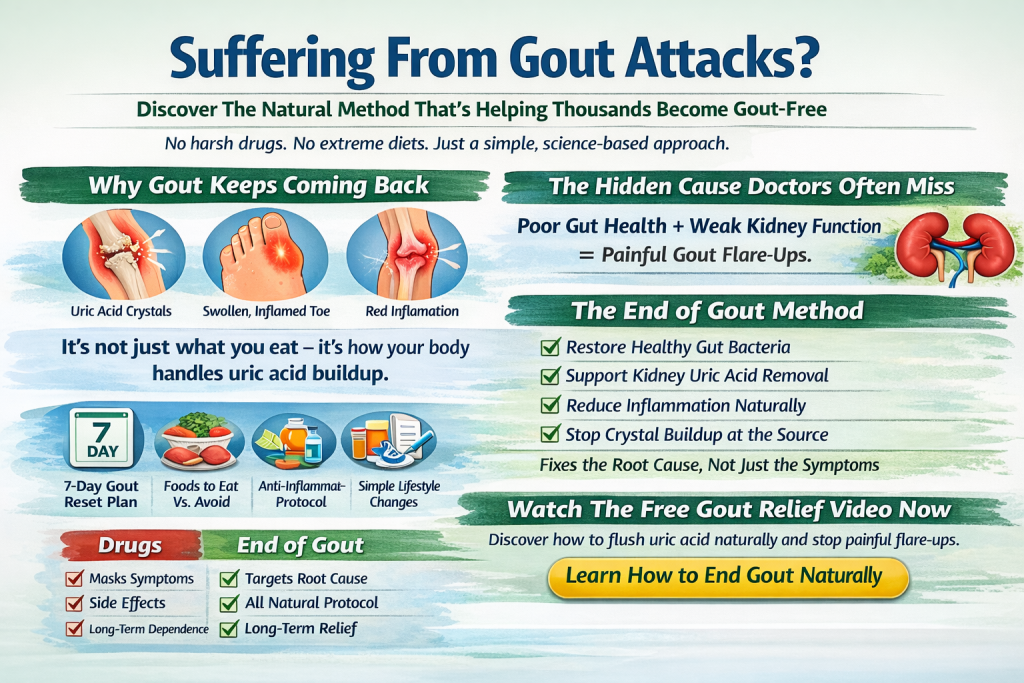
The condition itself is straightforward enough: uric acid crystals accumulate in joints, typically starting in the big toe, causing excruciating pain that sufferers often describe as feeling like shattered glass grinding inside the joint. But the psychological toll of living with gout extends well beyond these acute attacks.
The Pain-Depression Connection
The relationship between chronic pain and mental health is well-established, and gout fits squarely within this pattern. During flare-ups, the pain can be so severe that even the weight of a bedsheet becomes unbearable. Men experiencing these episodes often find themselves unable to work, care for their families, or engage in activities that give their lives meaning and structure.
This forced inactivity, combined with unrelenting pain, creates fertile ground for depression. Studies have found that men with gout are significantly more likely to experience depressive symptoms compared to those without the condition. The unpredictability of attacks adds another layer of psychological distress—never knowing when the next flare-up will strike can generate persistent anxiety and hypervigilance about one’s body.
Masculinity and the Shame Factor
For many men, gout carries an additional burden: shame. The condition has historically been associated with overindulgence—too much rich food, too much alcohol, and too much of the good life. While modern medicine understands that gout has complex genetic and metabolic causes beyond lifestyle choices, the stigma persists.
Men may feel judged by others or blame themselves for their condition, viewing it as a personal failure rather than a medical issue. This self-criticism can be particularly damaging for mental health. The stereotype of gout as a “disease of kings” or a result of gluttony can make men reluctant to discuss their condition openly, leading to social isolation at precisely the moment when support is most needed.
The Disability Dilemma
Gout can significantly impair mobility and function, especially during acute attacks or when the condition becomes chronic. For men whose identity is closely tied to their physical capabilities—whether through work, sports, or being the family provider—this loss of function can trigger an identity crisis.
The inability to perform tasks that once came easily, from playing with children to completing work projects, can erode self-esteem. When gout affects the feet or knees, even walking becomes a challenge. This limitation on independence can feel emasculating in cultures where male identity is connected to strength and self-sufficiency.
Sleep Disruption and Mental Health
Gout attacks often occur at night, waking sufferers from sleep with sudden, intense pain. Beyond the immediate discomfort, this pattern disrupts sleep architecture and leads to chronic sleep deprivation. The relationship between poor sleep and mental health is bidirectional—lack of sleep worsens mood and anxiety, while depression and anxiety make quality sleep more elusive.
Men with gout frequently report lying awake, dreading the next attack, or being unable to find a comfortable position. This chronic sleep disruption contributes to irritability, difficulty concentrating, and worsening depressive symptoms.
Social Withdrawal and Relationship Strain
The fear of triggering an attack can lead men to avoid social situations, particularly those involving alcohol or rich foods. Declining invitations repeatedly can strain friendships and lead to social isolation. Men may withdraw from social activities not just out of fear of dietary triggers, but also because they’re embarrassed about their condition or worried about having an attack in public.
Romantic relationships can suffer as well. Sexual activity may become difficult or impossible during flare-ups, and the chronic nature of the condition can place strain on partners who must take on additional responsibilities. The emotional distance that develops when one partner is dealing with chronic pain and the other feels helpless to provide relief can erode intimacy over time.
The Medication Burden
Managing gout typically requires long-term medication, and for some men, this represents another psychological challenge. Taking daily medication can serve as a constant reminder of the condition and feel like an admission of weakness or aging. Some men struggle with medication adherence, either due to side effects or a psychological resistance to accepting their chronic condition.
The need to make permanent lifestyle changes—reducing alcohol, modifying diet, losing weight—can feel overwhelming and contribute to feelings of deprivation and resentment, particularly when these changes don’t guarantee the elimination of attacks.
Breaking the Cycle
Recognizing the mental health impact of gout is the first step toward addressing it. Healthcare providers treating gout should routinely screen for depression and anxiety, understanding that managing the psychological aspects of the condition is as important as controlling uric acid levels.
For men with gout, several strategies can help protect mental health. Open communication with healthcare providers about both physical and emotional symptoms allows for comprehensive treatment. Connecting with support groups, either in person or online, can reduce the isolation and shame that often accompany the condition. These communities provide practical advice for managing symptoms while also offering emotional support from people who truly understand the experience.
Cognitive-behavioral approaches can help men reframe their relationship with gout, moving from self-blame to self-compassion and from catastrophizing about attacks to developing coping strategies. Working with a mental health professional who understands chronic pain conditions can provide tools for managing the emotional impact of the disease.
Physical activity, adapted to current capabilities, remains important for both physical and mental health. Swimming, cycling, or other low-impact exercises can be continued even when weight-bearing activities are difficult, providing mood benefits and a sense of agency over one’s health.
The Path Forward
Gout’s impact on men’s mental health deserves greater recognition in both clinical settings and public discourse. The condition is not merely a source of physical pain but a challenge that touches every aspect of life—work, relationships, self-image, and emotional well-being.
By acknowledging this broader impact and addressing mental health proactively, men with gout can reclaim a sense of control and quality of life. The goal isn’t just to reduce uric acid levels or prevent the next attack but to support the whole person navigating life with a chronic condition. When both body and mind receive attention and care, men with gout can move beyond mere survival to genuine thriving.