I. Introduction: The Knee’s Natural “Shock Absorber”
Articular cartilage is the smooth, tough, and low-friction protective covering that lines the ends of the bones in your joints. In a healthy knee, this tissue acts as a vital shock absorber, allowing the femur, tibia, and patella to glide over each other effortlessly and painlessly during daily activities and sports.
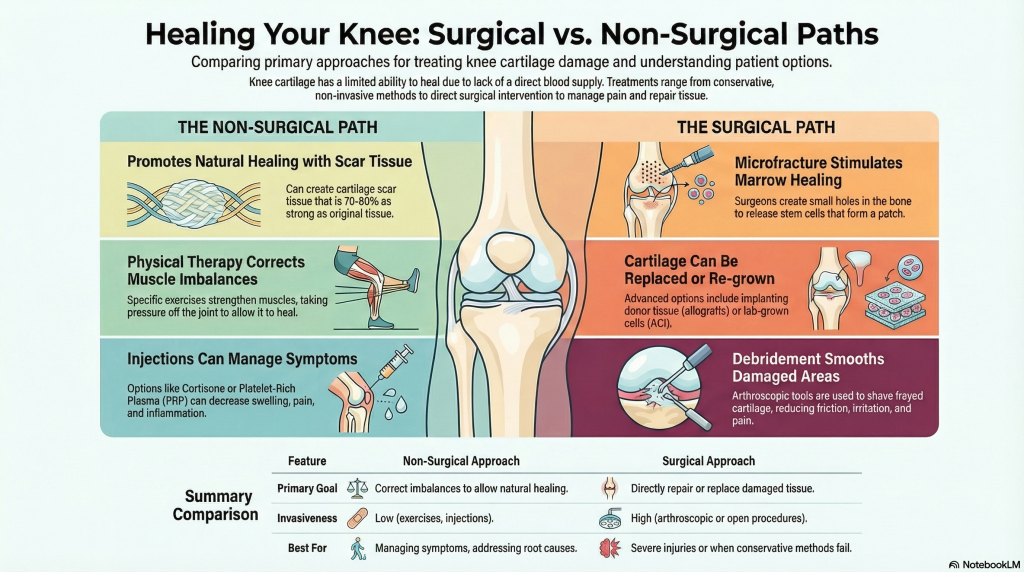
However, cartilage faces a significant biological hurdle: it has no direct blood supply. Unlike skin or bone, which receive nutrients through the bloodstream to repair damage, cartilage has little to no ability to heal itself naturally. To understand recovery, it is essential to distinguish between regeneration—the experimental process of growing 100% brand-new, identical cells—and healing, which involves the body filling defects with fibrocartilage (scar tissue).
We want to share some encouraging news: yes, your knee cartilage can heal, even if you have been diagnosed with a “bone-on-bone” condition. While cartilage lacks a direct blood supply and cannot fix itself naturally, it can heal by developing fibrocartilage (scar tissue) that is approximately 70% to 80% as durable as your original tissue. By correcting muscle imbalances to offload joint pressure or utilizing advanced regenerative therapies like PRP and stem cell treatments, you can often “renew” your joint and avoid a total replacement.
We have much more to share with you below, including the specific “pre-hab” exercises you can start today and the breakthrough medical technologies that are making knee renewal more successful than ever before.
II. Identifying the Damage: Symptoms and Diagnosis
Cartilage damage can occur through traumatic injury (like a fall or twist) or through gradual wear and tear known as osteoarthritis.
- Recognizing the Signs: Most patients report a constant, dull ache and swelling that worsens with activity. You may also notice “crunchy sounds” or stiffness, particularly in the morning or after sitting for long periods.
- Mechanical Symptoms: If a piece of cartilage breaks off and becomes a “loose body” floating in the joint, it can cause the knee to “lock” or “catch” during movement.
- The Diagnostic Toolkit: While X-rays provide a “snapshot” of the joint, they primarily show bones and the space between them; they cannot directly see cartilage or the meniscus. To confirm a cartilage injury, a doctor will typically order an MRI or CT scan to see the actual soft tissue damage.
III. The “Bone-on-Bone” Myth: Is Healing Still Possible?
Many patients are told they are “bone-on-bone,” implying a total joint replacement is the only option. However, it is absolutely possible for cartilage to heal even in these situations.
- Positional vs. Permanent: An X-ray is a single moment in time. The space between your bones changes as you move. Often, muscle imbalances pull the joint into a compressed position that looks “bone-on-bone”.
- Normalizing the Joint: By altering these muscle forces through specific exercises, you can “offload” the pressure on the worn-down spot.
- The 70-80% Rule: When the pressure is removed, the body can fill in the damaged area with scar tissue. This fibrocartilage is roughly 70% to 80% as durable as the original tissue, which is often enough to restore function and eliminate pain.
IV. Non-Surgical Restoration: Fix the Mechanics
The goal of non-surgical restoration is to improve circulation and correct muscle imbalances. The most common issue is quad-dominance, where overly strong quadriceps pull the kneecap too tightly against the thigh bone, accelerating wear.
The “Pre-hab” Protocol:
- Improve Circulation: Simple movements like ankle pumps (pressing like a gas pedal) and “windshield wipers” (rotating the foot side-to-side) help pump fluid and lubrication into the joint.
- Strengthening Stability:
- Straight Leg Raises: Lying on your back and raising the leg helps strengthen the quads without grinding the joint.
- Towel Presses: Placing a rolled-up towel under the knee and pressing down activates the quadriceps and their tendons.
- Wall Sits (Wall Squats): This isometric exercise strengthens the glutes and core, which are essential for hip and knee stabilization.

V. Advanced Surgical Options: Beyond Simple Debridement
If non-surgical methods are insufficient, several “knee renewal” techniques can address localized defects:
- Debridement: This involves using arthroscopic instruments to “shave” and smooth frayed cartilage to reduce friction.
- Microfracture: The traditional standard where surgeons create small holes in the bone to allow blood and marrow to stimulate the growth of a scar tissue patch.
- Biocartilage Grafting: A newer technique that improves on microfracture by using a paste of micronized cartilage mixed with Platelet-Rich Plasma (PRP) to encourage the growth of real articular cartilage rather than just scar tissue.
- OATS (Osteochondral Autograft Transplantation): Moving a plug of healthy cartilage and bone from a non-weight-bearing area to the damaged site.
- MACI (Matrix-induced Autologous Chondrocyte Implantation): A two-step process where your own cells are grown in a lab on a scaffold and then re-implanted into the knee.
Special: Joint Pain? Eat THIS Nutrients…More HERE
VI. Regenerative Medicine: The Future of Orthopaedics
Regenerative medicine aims to stimulate the body’s natural healing response through biologics.
- Platelet-Rich Plasma (PRP): Concentrated platelets from your own blood are injected into the knee to deliver growth factors that reduce inflammation and improve symptoms.
- Stem Cell Therapy: Doctors are exploring AMAT/MFAT (microfragmented fat) and bone marrow aspirates, which contain stem cells and pericytes that can significantly improve pain and function.
- The NITRO Program: This five-year research initiative is developing “healing shots,” injury-patching hydrogels, and annual infusions designed to stop bone erosion and kick-start cartilage regrowth.
VII. Taking the First Step
Healing a knee is not an immediate process; cartilage has a low metabolism, and changes often take a few weeks to become noticeable. However, by focusing on joint preservation through mechanical correction and modern biologics, many patients can avoid or significantly delay a total joint replacement.
The “Pothole” Analogy: Think of your knee like a road. If the entire road is disintegrated, you have to pave over it completely (joint replacement). But if the damage is just a single “pothole,” modern medicine allows us to patch that specific spot with a “repair kit”—whether through exercise, scar tissue, or advanced grafting—to restore a smooth driving surface (cartilage restoration).
Based on the sources provided, here is a comprehensive list of frequently asked questions and answers for individuals researching knee cartilage healing and restoration.
General Understanding and Biology
What exactly is articular cartilage, and why is it important? Articular cartilage is a smooth, tough, and flexible connective tissue that covers the ends of bones in a joint. Its primary role is to act as an effective shock absorber and a low-friction surface, allowing your knee to move easily and painlessly.
Can cartilage heal on its own? Natural healing is extremely limited because cartilage has no direct blood supply. When other tissues like bone or skin are injured, the body sends nutrients through the blood to repair them, but cartilage is “out of luck” in this regard.
What is the difference between “healing” and “regeneration”? Regeneration refers to growing brand-new cells that are identical to the original tissue, which is currently considered experimental. Healing is what occurs naturally when the body puts down scar tissue (fibrocartilage) to fill a defect. This scar tissue is typically 70% to 80% as durable as the original tissue.
Symptoms and Diagnosis

What are the common signs of a cartilage injury? The most frequent complaints include a constant dull ache and swelling during or after activity. You may also experience “crunchy” sounds (crepitus) or stiffness, particularly in the morning or after sitting for a long time.
Why does my knee “lock” or “catch”? This is often caused by “loose bodies,” which are pieces of cartilage that have broken off from the bone and are floating within the joint. They can become lodged in the joint during motion, causing it to catch.
If my doctor says I am “bone-on-bone,” can I still heal? Yes. A “bone-on-bone” diagnosis on an X-ray is often a snapshot in time that may be caused by muscle imbalances pulling the joint together. By correcting these imbalances and offloading the pressure, the joint space can normalize, allowing the area to fill with protective scar tissue.
Why do I need an MRI if I already had an X-ray? X-rays primarily show bones and the space between them; they cannot show cartilage, the meniscus, or tendons. An MRI or CT scan is necessary to see the actual soft tissue damage.
Non-Surgical Management and Exercise
How can I heal my knee without surgery? Non-surgical healing focuses on improving circulation and fixing muscle imbalances. Strengthening the muscles that stabilize the knee takes tension and pressure off the damaged cartilage, creating a “healing environment”.
What is the most common muscle imbalance affecting the knee? The most common issue is “quad dominance,” where the quadriceps (front thigh muscles) are too strong or tight. This can pull the kneecap too hard against the thigh bone or compress the joint, wearing down cartilage and the meniscus over time.
Special: Joint Pain? Eat THIS Nutrients…More HERE
What exercises are recommended for knee restoration?
- For Circulation: Ankle pumps and “windshield wiper” foot movements.
- For Strengthening: Straight leg raises, wall sits (wall squats) to activate glutes and core, and towel presses under the knee to activate the quads and tendons.
- For Stability: Side-lying leg raises (clamshells) to target the abductors and glutes.
Advanced and Regenerative Treatments
What are the standard surgical options for cartilage repair?
- Debridement: Shaving and smoothing frayed cartilage to reduce friction.
- Microfracture: Creating tiny holes in the bone to stimulate marrow and grow a scar tissue patch.
- OATS (Osteochondral Autograft): Moving a unit of healthy cartilage and bone from a non-weight-bearing area to the damaged site.
- MACI (Matrix-induced Autologous Chondrocyte Implantation): Growing your own cartilage cells in a lab and re-implanting them into the knee.
What is PRP (Platelet-Rich Plasma)? PRP involves drawing your own blood, concentrating the platelets, and injecting them into the joint. The growth factors and anti-inflammatory proteins in the platelets can improve symptoms and boost healing, though it may not “regrow” original tissue.
What is the “NITRO” program? NITRO is a high-level research project aiming to develop “healing shots,” injury-patching hydrogels, and annual infusions within the next five years to stop bone erosion and kick-start cartilage regrowth.
Analogy for Understanding Treatment: To understand the difference between fixing a specific injury versus a total replacement, think of your knee like a pothole in a road. If the entire road is disintegrated, you must repave the whole thing (joint replacement). However, if there is just a single hole, modern medicine allows you to use a “repair kit” to patch that specific spot, restoring a smooth driving surface (cartilage restoration).
A Practical Next Step
If you’re serious about protecting your knees and avoiding unnecessary surgery, having the right support tools matters. I don’t believe in miracle products—but I do believe in using proven joint-support options that make movement easier while you work on strength, mobility, and inflammation control.
I’ve personally reviewed a few joint-support and knee-care resources that can help reduce stress on the knee and support long-term joint health. They’re not replacements for smart movement or lifestyle changes—but they can make the process easier and more sustainable.
If you want to explore those options, check the video here
That’s it. No pressure. No hype. Just guidance.